What is Skin Pigmentation?
Skin pigmentation refers to the colouration of the skin, primarily determined by the presence and distribution of a pigment called melanin. Melanin is produced by specialized cells called melanocytes, located in the outermost layer of the skin known as the epidermis. The amount and type of melanin in the skin determine its color, which can vary from very light to very dark.
The main function of melanin is to protect the skin from the harmful effects of ultraviolet (UV) radiation from the sun. When the skin is exposed to sunlight, the production of melanin increases as a protective mechanism. This is why people living in regions with intense sunlight tend to have darker skin tones, as their skin produces more melanin to shield against excessive UV exposure.
There are three main categories of skin pigmentation:
- Eumelanin:
Responsible for dark skin colors, such as brown or black where people with higher levels of eumelanin tend to have darker skin tones. - Pheomelanin:
Responsible for lighter skin colors, such as red or yellow. It does not provide as much protection against UV radiation as eumelanin. - Mixed Melanin:
Many individuals have a combination of eumelanin and pheomelanin in their skin, resulting in various intermediate skin tones.
The distribution and amount of melanin in the skin are influenced by a combination of genetic factors and environmental factors, particularly sun exposure. People from different ethnic backgrounds tend to have specific skin pigmentation characteristics, but there is a wide range of skin tones within each ethnic group.
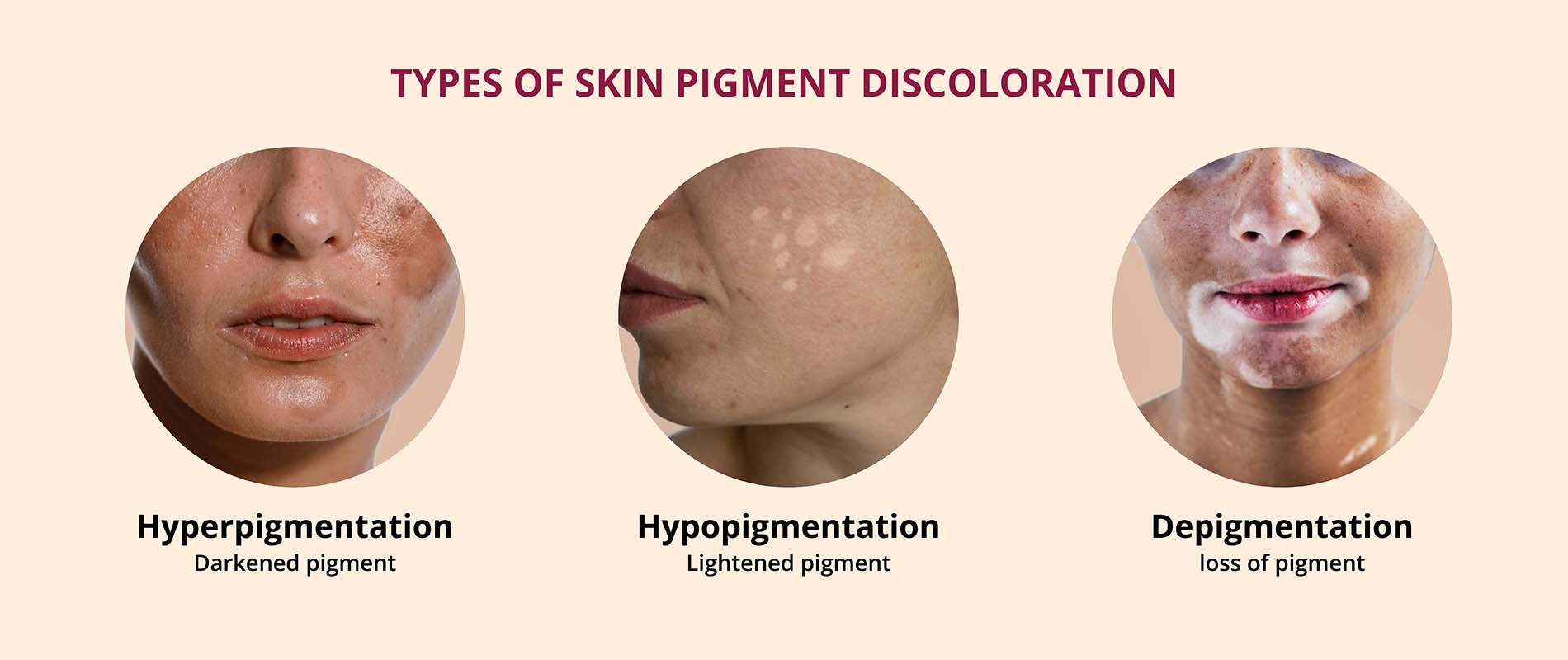
Imbalances in skin pigmentation can lead to various conditions, such as:
- Hyperpigmentation:
When certain areas of the skin become darker than the surrounding skin due to an increase in melanin production, caused by factors like sun exposure, hormonal changes, skin injuries or certain medications. - Hypopigmentation:
Areas of the skin that become lighter than the surrounding skin due to a decrease in melanin production. Conditions like vitiligo result from the loss of melanocytes, leading to white patches on the skin.
Also Read : Why Does Pigmentation Happen? And Different Types Of Pigmentation?
Understanding Melanin and Its Role
Melanin is a complex pigment responsible for the coloration of various tissues in the body, including the skin, hair, and eyes, produced by specialized cells called melanocytes found in the skin’s outermost layer, the epidermis. The production and distribution of melanin play a crucial role in determining an individual’s skin color.
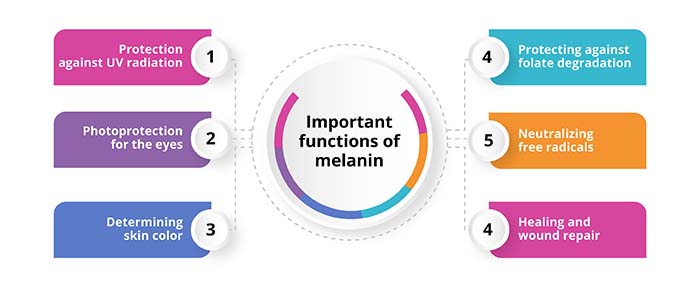
Important functions of Melanin
Protection against UV radiation
When the skin is exposed to sunlight, melanocytes release melanin into the surrounding skin cells.
Acts as a natural sunscreen, absorbing and dissipating UV radiation, thus reducing the risk of DNA damage and skin cancer caused by excessive sun exposure.
Photoprotection for the eyes
Melanin is also present in the eyes, where it helps protect the retina from damage caused by UV radiation.
The amount of melanin in the eyes affects their color, with more melanin resulting in darker eye colors.
Determining skin color
The type and amount of melanin in the skin determine an individual’s skin color.
- Eumelanin – responsible for brown and black pigmentation, provides a higher level of UV protection
- Pheomelanin – responsible for red and yellow pigmentation, offers less protection against UV radiation
Healing and wound repair
Melanin is involved in reducing inflammation and promoting tissue repair after skin injuries.
Neutralizing free radicals
Antioxidant properties help to neutralize free radicals that can damage cells and contribute to aging and various health issues.
Protecting against folate degradation
Serves to protect the body’s stores of folate (a B vitamin essential for cell division and development) from degradation by UV radiation.
The amount and distribution of melanin in the skin are determined by a combination of genetic and environmental factors. People with higher levels of eumelanin tend to have darker skin tones, while those with higher levels of pheomelanin tend to have lighter skin tones. While melanin provides important photoprotective benefits, it is not a complete shield against all harmful effects of UV radiation. Sunscreen and other protective measures are still essential to prevent skin damage and reduce the risk of skin cancer.
Types of Skin Pigmentation Disorders
Skin pigmentation disorders are a group of conditions that affect the coloration of the skin, leading to either darkening or lightening of certain areas. These disorders result from imbalances in the production, distribution, or function of the pigment melanin, which is responsible for skin color. Melanin is produced by specialized cells called melanocytes and helps protect the skin from the harmful effects of UV radiation.
Hyperpigmentation
Hyperpigmentation is a common skin condition characterized by the darkening of certain areas due to an excess production of melanin, of the skin compared to the surrounding skin. While harmless, it can be a source of concern for many individuals due to its impact on appearance.
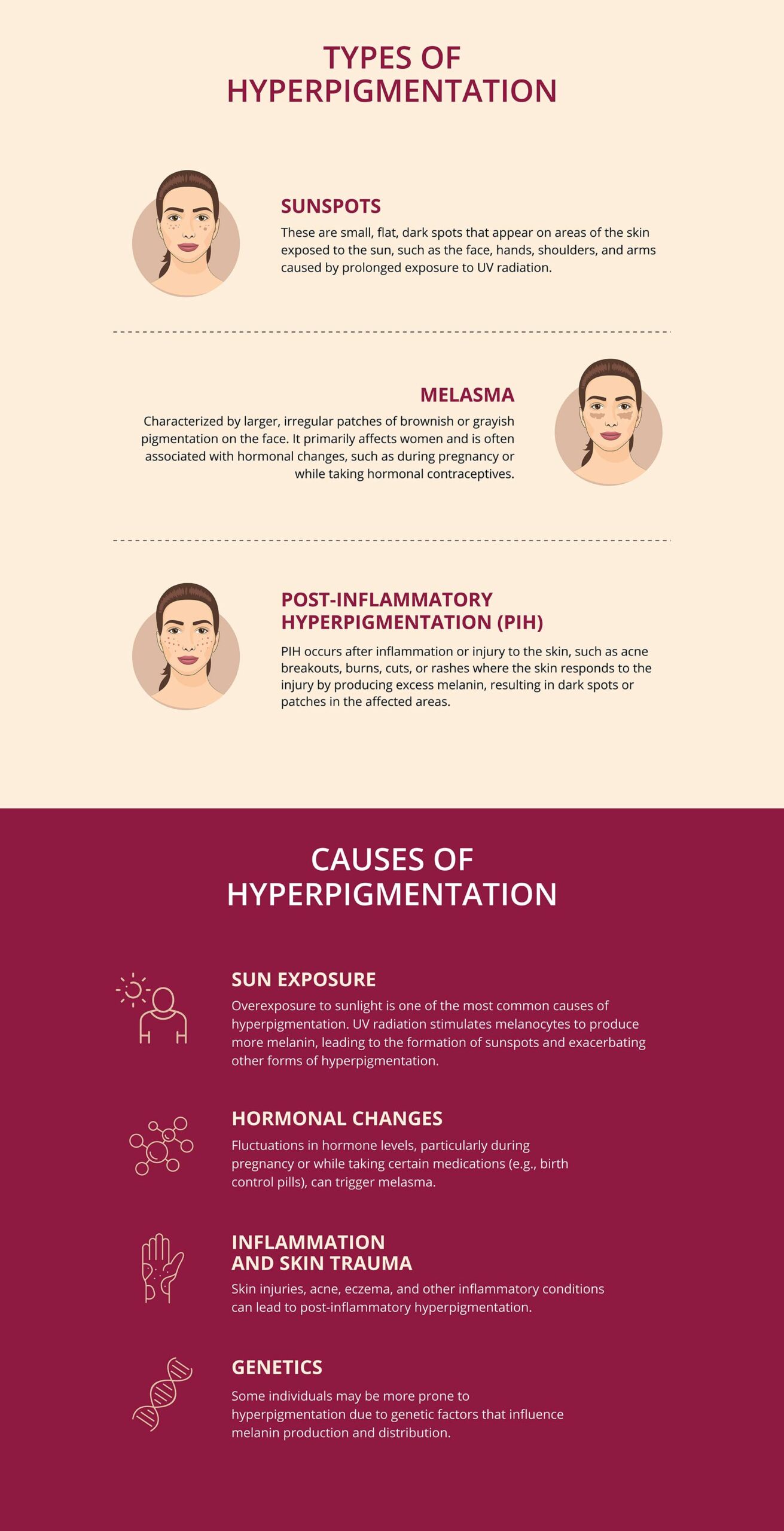
Types of Hyperpigmentation
Sunspots
These are small, flat, dark spots that appear on areas of the skin exposed to the sun, such as the face, hands, shoulders, and arms caused by prolonged exposure to UV radiation.
Melasma
Characterized by larger, irregular patches of brownish or grayish pigmentation on the face. It primarily affects women and is often associated with hormonal changes, such as during pregnancy or while taking hormonal contraceptives.
Post-inflammatory Hyperpigmentation (PIH)
PIH occurs after inflammation or injury to the skin, such as acne breakouts, burns, cuts, or rashes where the skin responds to the injury by producing excess melanin, resulting in dark spots or patches in the affected areas.
Causes of Hyperpigmentation
Sun exposure
Overexposure to sunlight is one of the most common causes of hyperpigmentation. UV radiation stimulates melanocytes to produce more melanin, leading to the formation of sunspots and exacerbating other forms of hyperpigmentation.
Hormonal changes
Fluctuations in hormone levels, particularly during pregnancy or while taking certain medications (e.g., birth control pills), can trigger melasma.
Inflammation and skin trauma
Skin injuries, acne, eczema, and other inflammatory conditions can lead to post-inflammatory hyperpigmentation.
Genetics
Some individuals may be more prone to hyperpigmentation due to genetic factors that influence melanin production and distribution.
Treatment Options
Chemical peels
Involve applying a chemical solution to the skin, which causes the top layer to peel off, revealing fresher, less pigmented skin underneath.

Q switch laser
Target the melanin in the skin to break up the excess pigment, leading to a more even skin tone.

Check more on skin treatment options
Hypopigmentation
Hypopigmentation is a skin condition characterized by the loss or reduction of melanin, the pigment responsible for skin color; as a result of which areas of the skin affected by hypopigmentation appear lighter or white compared to the surrounding skin. This occurs due to a decrease in the number of melanocytes (the cells that produce melanin) or a reduction in melanin synthesis within these cells.
Types of Hypopigmentation
Vitiligo
An autoimmune disorder where the body’s immune system attacks and destroys melanocytes, leading to the development of white patches on the skin. These patches can appear on various parts of the body and may gradually spread over time.
Albinism
A genetic condition that affects the production of melanin in the body, as a result of which individuals have very light skin, hair, and often have pink or red eyes due to the lack of pigment in the irises.
Tinea Versicolor
A fungal infection that can cause hypopigmentation or hyperpigmentation on the skin. In the case of hypopigmentation, the affected areas appear lighter.
Post-inflammatory Hypopigmentation
Like post-inflammatory hyperpigmentation, inflammation or injury to the skin can also lead to hypopigmentation where certain skin conditions or treatments such as burns, rashes, or dermatological procedures cause the skin to lose its pigment temporarily.
Causes of hypopigmentation
Genetics
Autoimmune response
Fungal infections
Inflammation and injury
Treatment options
Phototherapy
Light-based treatments, such as narrowband UVB therapy, may help stimulate melanocytes and repigment the affected areas in some cases of vitiligo.
Micropigmentation
Also known as medical tattooing, micropigmentation involves depositing pigment into the skin to match the surrounding areas and create a more uniform appearance.
Melasma

Melasma is a common chronic skin condition characterized by the development of brownish or grayish patches on the face, particularly on the cheeks, forehead, upper lip, and chin. It primarily affects women and is often referred to as “chloasma” or the “mask of pregnancy” when it occurs during pregnancy, as hormonal changes can trigger its onset.
Causes of Melasma
Hormonal changes
Hormonal fluctuations, particularly increased levels of estrogen and progesterone, play a significant role in triggering melasma. Pregnancy, oral contraceptive use and hormone replacement therapy can all be contributing factors.
Sun exposure
Ultraviolet (UV) radiation from the sun is a key trigger for melasma. Sunlight stimulates the production of melanin in the skin, and individuals with melasma are more sensitive to the effects of sunlight, leading to the formation of darker patches.
Genetics
A family history of melasma or other pigmentation disorders may increase an individual’s susceptibility to developing the condition.
Ethnicity
People with darker skin tones, particularly those of Asian, Hispanic or African descent, are more prone to melasma.
Certain medications and cosmetics
Some medications, such as those containing hormones or certain photosensitizing agents, can trigger or worsen melasma. Additionally, the use of cosmetics or skincare products that irritate the skin may exacerbate the condition.
Treatment options for Melasma:
Sun protection
Broad-spectrum sunscreen with a high SPF, protective clothing, and seeking shade during peak sunlight hours can help prevent further darkening of the affected areas.
Topical agents
Topical creams or lotions containing ingredients such as hydroquinone, tretinoin, corticosteroids, azelaic acid or kojic acid help lighten the pigmented patches and inhibit melanin production.
Chemical peels
Application of a chemical solution to exfoliate the top layer of the skin, promoting the growth of new, less pigmented skin cells.
Laser and Light therapies
Laser and intense pulsed light (IPL) treatments can target the melanin in the affected areas, breaking up the excess pigment and reducing the appearance of melasma.
Combination therapies
A combination of treatments, such as topical agents and laser therapy, may be more effective in managing melasma than a single treatment approach.
Vitiligo

Vitiligo is a chronic skin disorder characterized by the loss of melanocytes, the cells responsible for producing melanin. As a result, individuals with vitiligo develop patches of depigmented or white skin on various parts of their bodies. The condition can affect people of all ages, genders, and ethnicities and its exact cause is not fully understood.
Types of Vitiligo
Depigmented patches
Vitiligo is characterized by the appearance of well-defined, milky-white patches on the skin. These patches may vary in size and shape and can occur symmetrically on both sides of the body.
Affected body areas
The patches of vitiligo can appear on any part of the body, but they often occur in areas exposed to the sun, such as the face, hands, feet, arms, and genital area. Other common sites include the knees, elbows, and around body openings (e.g., eyes, nostrils, mouth).
There are different types of vitiligo, classified based on the distribution and pattern of depigmented patches. These types include generalized (most common), segmental (affecting one side or segment of the body), focal (limited to a few small areas), and acrofacial (affects the face and extremities).
Causes and risk factors
The exact cause of vitiligo is not fully understood, but several factors are believed to play a role:
Autoimmune response
The body’s immune system mistakenly attacks and destroys its own melanocytes, leading to the loss of pigment.
Genetic predisposition
It tends to run in families where certain genes may increase an individual’s susceptibility to the condition.
Oxidative stress
Some researchers believe that oxidative stress, caused by an imbalance between free radicals and antioxidants in the body, may contribute to the destruction of melanocytes.
Environmental triggers
Exposure to certain chemicals or stress, may trigger or exacerbate vitiligo in individuals who are genetically predisposed.
Treatment options
While there is no cure for vitiligo, several treatment options are available to manage the condition and improve its appearance:
Topical corticosteroids
These creams or ointments can help reduce inflammation and repigment the skin in some cases of vitiligo.
Topical calcineurin inhibitors
These medications can be used to suppress the immune response and help restore pigment to the affected areas.
Phototherapy
Light-based treatments, such as narrowband UVB or PUVA (psoralen plus ultraviolet A), can stimulate melanocyte activity and promote repigmentation.
Depigmentation
In cases of extensive vitiligo, where repigmentation is not feasible, depigmentation therapy using topical agents may be considered to even out the skin color.
Surgical procedures
Surgical interventions, such as skin grafting, melanocyte transplantation, and tattooing, may be used to repigment the affected areas.
It’s important to note that the effectiveness of treatments varies from person to person, and some treatments may have side effects.
Living with Vitiligo
Vitiligo can have a significant emotional and psychological impact on affected individuals due to the changes in appearance it brings. Coping with vitiligo may involve a combination of medical treatment, sun protection to prevent sunburn on depigmented areas, and support from mental health professionals or vitiligo support groups.
Albinism

Albinism is a congenital genetic disorder characterized by the partial or complete absence of melanin, the pigment responsible for skin, hair, and eye color. It occurs due to inherited gene mutations that affect the production or distribution of melanin in the body. Individuals with albinism have very little or no melanin in their skin, hair, and eyes, leading to a distinct appearance and certain visual impairments.
Characteristics of Albinism
Hypopigmentation
The hallmark feature of albinism is the significant reduction or absence of melanin in the skin, hair, and eyes. Individuals with albinism have very light skin, ranging from white to light pinkish, and their hair can be white, light blond, or light brown.
Ocular features
Albinism often affects the eyes, leading to various visual impairments such as nystagmus (involuntary eye movements), strabismus (crossed eyes) and photophobia (sensitivity to light). The lack of pigment in the eyes also causes iris translucency, giving the irises a light blue, gray, or even reddish appearance, as the underlying blood vessels show through.
Visual impairments
Reduced visual acuity, decreased depth perception,difficulty with fine detail tasks, many also have a condition called foveal hypoplasia, where the central part of the retina (fovea) is underdeveloped, leading to poor central vision.
Types of Albinism
- Oculocutaneous Albinism (OCA):
Characterized by reduced melanin in the skin, hair, and eyes. - Ocular Albinism (OA):
Reduction of melanin primarily in the eyes, leading to visual impairments. The skin and hair color may be closer to that of unaffected individuals.
Causes of Albinism
Albinism is a genetic condition, meaning it is inherited from one or both parents who carry the mutated genes responsible for the disorder.
- Management and Support:
There is no cure for albinism, but various interventions can help manage its effects and improve the quality of life for individuals with the condition: - Visual aids:
Eyeglasses, contact lenses, or low vision aids can assist individuals with albinism in improving their visual acuity and managing light sensitivity. - Sun protection:
Sunscreen, protective clothing, and staying in the shade are essential for preventing harmful effects of UV radiation. - Vision therapy:
Vision therapy can help to enhance eye coordination and visual processing skills. - Education and support:
Early intervention, special education, and support groups can help cope with the challenges associated with the condition.
Post-Inflammatory Hyperpigmentation (PIH)

Post-Inflammatory Hyperpigmentation (PIH) is a common skin condition characterized by dark patches or spots that develop on the skin after an inflammatory injury or trauma. It occurs when the skin produces an excess of melanin in response to inflammation, leading to localized areas of increased pigmentation. PIH is more prevalent in individuals with darker skin tones.
Causes of Post-Inflammatory Hyperpigmentation:
- Acne:
After an acne lesion heals, it can leave behind dark marks. - Skin injuries:
Cuts, burns, insect bites or any other injury that affects the skin’s integrity can trigger an inflammatory response and lead to PIH. - Allergic reactions:
Inflammation resulting from allergic reactions to certain substances or chemicals can also cause PIH. - Skin disorders:
Conditions like eczema, psoriasis, and lichen planus, which involve inflammation of the skin, can leave behind hyperpigmented spots as they heal. - Dermatological procedures:
Chemical peels, dermabrasion, or laser treatments, can cause temporary PIH during the healing process.
Characteristics of Post-Inflammatory Hyperpigmentation
- Pigment variations:
PIH presents as dark spots or patches that are typically brown, black or grayish in colour and may vary in intensity and size, depending on the extent of inflammation and individual skin response. - Temporary condition:
Generally temporary and fades over time, although it may take weeks to several months for the discoloration to improve. - Localization:
The darkened areas are often limited to the specific sites of the previous inflammatory event, such as the locations of previous acne breakouts or skin injuries.
Treatment Options for Post-Inflammatory Hyperpigmentation
PIH usually resolves on its own, but several treatments can help expedite the fading process and improve skin appearance, such as:
Topical lightening agents:
Over-the-counter or prescription creams containing ingredients like hydroquinone, retinoids, kojic acid, azelaic acid, or vitamin C can help lighten the dark spots and even out the skin tone.
- Chemical peels:
Use of mild acids in chemical peels can exfoliate the skin’s top layer, promoting the growth of new, less pigmented skin cells. - Laser and light therapies:
Laser treatments and intense pulsed light (IPL) can target the excess melanin in the affected areas, breaking it down and reducing pigmentation. - Sun protection:
Sunscreen with a high SPF is crucial to protect the skin from UV radiation, as exposure to the sun can worsen PIH and delay the fading process. - Prevention:
Preventing PIH involves managing and minimising skin inflammation and avoiding picking or squeezing acne lesions. Early and effective treatment of inflammatory skin conditions and skin injuries can also help reduce the likelihood of developing PIH. Sun protection is crucial to prevent worsening of hyperpigmentation and to promote overall skin health.
What Causes Skin Pigmentation Issues?
Skin pigmentation issues can arise from various factors, including genetic, environmental, and medical influences. The skin’s colour is primarily determined by the amount and distribution of melanin, the pigment produced by melanocytes (specialised skin cells). Too much or too little melanin can result in different pigmentation issues.
- Genetics:
The most fundamental factor in skin colour is genetics. Different ethnicities have varying levels of melanin production, which is inherited from one’s parents. - Sun Exposure:
Ultraviolet (UV) radiation from the sun stimulates melanocytes to produce melanin as a protective response. Prolonged and excessive sun exposure can lead to an increase in melanin production, resulting in tanning. - Hormonal Changes:
Hormonal fluctuations can influence melanin production, leading to various pigmentation issues. - Post-Inflammatory Hyperpigmentation (PIH):
Skin inflammation caused by acne, wounds, rashes, or skin disorders can trigger the overproduction of melanin in the affected area, leading to dark spots or patches. - Skin Disorders:
Certain skin conditions, such as vitiligo (loss of melanocytes), albinism (lack of melanin production), and various types of hyperpigmentation disorders, are caused by genetic mutations affecting melanin production or distribution. - Age:
As people age, the natural production of melanin can decrease, leading to a loss of skin pigmentation and the development of age spots or grey hair. - Medications:
Some medications, such as certain antibiotics, antimalarial drugs, or chemotherapeutic agents, can cause changes in skin pigmentation as a side effect. - Skin Trauma:
Injuries to the skin, such as burns, cuts, or surgery, can sometimes trigger irregular melanin production and result in post-traumatic hyperpigmentation or hypopigmentation. - Cosmetic and Skincare Products:
The use of certain cosmetics or skincare products, especially those with irritants or harsh chemicals, can cause skin irritation and pigmentation issues.
How can skin pigmentation be diagnosed?
Diagnosing skin pigmentation involves a comprehensive evaluation by a dermatologist or healthcare professional. The diagnosis is based on a combination of a physical examination, analysing medical history and at times additional tests to determine the underlying cause and type of pigmentation issue.
How skin pigmentation is typically diagnosed:
- Medical history:
A detailed medical history, including any past or current skin conditions, family history of pigmentation disorders, exposure to UV radiation or tanning beds, recent use of medications or skincare products, and any relevant symptoms experienced by the individual. - Physical examination:
Examination of the affected skin areas and the overall condition of the skin to assess the size, shape and colour of the pigmented areas, as well as the distribution and any other characteristics that may aid in the diagnosis. - Pattern recognition:
Dermatologists often rely on their experience and pattern recognition skills to identify common pigmentation issues, such as freckles, sunspots, melasma, and vitiligo. - Wood’s lamp examination:
In some cases, a Wood’s lamp (UV lamp) may be used during the examination. The lamp emits ultraviolet light, which can help highlight certain pigmentation disorders, such as vitiligo or fungal infections. - Biopsy:
In specific situations where the diagnosis is unclear or to rule out other skin conditions, a skin biopsy may be performed. During a biopsy, a small sample of the affected skin is removed and examined under a microscope. - Dermoscopy:
A non-invasive technique that allows dermatologists to examine pigmented skin lesions in more detail. It helps differentiate between benign and malignant lesions, aiding in the diagnosis of potential skin cancers. - Blood tests:
In some cases, blood tests may be conducted to check for underlying medical conditions that can cause pigmentation issues, such as hormonal imbalances. - Patch testing:
Patch testing may be performed to diagnose allergic contact dermatitis, a condition that can cause skin discoloration due to an allergic reaction.
Tips for Preventing Skin Pigmentation Issues
Preventing skin pigmentation issues involves adopting a combination of sun protection measures, a healthy lifestyle, and proper skin care practices. Some essential tips to help prevent skin pigmentation issues:
-
Sun protection:
- Use sunscreen-
Apply a broad-spectrum sunscreen with an SPF of 30 or higher daily, even on cloudy days. Reapply every two hours or more frequently if swimming or sweating. - Seek shade-
Limit direct sun exposure, especially during peak hours between 10am and 4pm, when the sun’s UV rays are strongest. - Wear protective clothing-
Cover up with long-sleeved shirts, wide-brimmed hats, and sunglasses that block UV rays. - Avoid tanning beds-
Avoid using tanning beds or sunlamps, as they emit harmful UV radiation and increase the risk of skin pigmentation issues and skin cancer.
- Use sunscreen-
-
Manage skin conditions:
- Treat acne promptly-
Early and effective treatment of acne can help prevent post-inflammatory hyperpigmentation (PIH). - Manage skin disorders-
If you have conditions like eczema, psoriasis, or lichen planus, work with a healthcare professional to manage them properly to minimise skin inflammation and pigmentation issues.
- Treat acne promptly-
-
Be gentle with your skin:
- Avoid picking or scratching-
Picking at acne or scabs can lead to skin trauma and PIH. - Gentle cleansing:
Use mild, non-abrasive cleansers to avoid irritating the skin.
- Avoid picking or scratching-
-
Hormonal management:
- Manage hormonal changes-
During pregnancy or while taking hormonal medications, consult a healthcare professional to address skin changes like melasma.
- Manage hormonal changes-
-
Stay hydrated:
Drink plenty of water to keep your skin hydrated and promote overall skin health.
-
Avoid harsh chemicals:
Be cautious with cosmetic products that may contain harsh chemicals, as they can irritate the skin and cause pigmentation issues.
-
Use sunless tanners:
If you want a tan appearance, consider using sunless tanning products (self-tanners) that do not involve UV radiation.
-
Healthy Lifestyle:
- Eat a balanced diet-
Consume a diet rich in fruits, vegetables, and antioxidants to support skin health. - Get regular exercise-
Regular physical activity promotes healthy circulation, which can benefit the skin. - Manage stress-
Chronic stress can contribute to skin issues, so practise stress-reducing activities like meditation or yoga. - Regular check-ups-
Visit a dermatologist for regular skin check-ups, especially if you have a history of pigmentation issues or a family history of skin cancer.
- Eat a balanced diet-
10 Natural remedies for skin pigmentation
Natural remedies for skin pigmentation can be used as complementary treatments to help lighten dark spots, even out skin tone, and promote healthy skin. While these remedies may not provide instant results like medical treatments, they can be effective over time and are generally safe for most skin types.
Some popular natural remedies for skin pigmentation are:
- Aloe vera gel:
Aloe vera has soothing and anti-inflammatory properties that can help fade dark spots and promote skin healing. Apply fresh aloe vera gel directly to the affected areas and leave it on for 20-30 minutes before rinsing off. - Lemon juice:
Lemon juice contains natural bleaching agents like citric acid, which can help lighten dark spots. Apply fresh lemon juice to the pigmented areas using a cotton ball and leave it on for about 10-15 minutes before rinsing off. Be cautious if you have sensitive skin, as lemon juice can cause irritation in some individuals. - Vitamin E oil:
Vitamin E oil has antioxidant properties that can help repair and protect the skin. Apply a few drops of vitamin E oil directly to the dark spots and gently massage it into the skin. - Turmeric:
Turmeric has anti-inflammatory and antioxidant properties that can help improve skin pigmentation. Make a paste by mixing turmeric powder with milk or water and apply it to the affected areas. Leave it on for 15-20 minutes before rinsing off. - Honey:
Honey has moisturising and healing properties that can benefit the skin. Apply raw honey to the pigmented areas and leave it on for 20-30 minutes before rinsing off. - Papaya:
Papaya contains enzymes and natural exfoliants that can help lighten dark spots and promote skin renewal. Mash ripe papaya and apply it as a mask to the pigmented areas for 15-20 minutes before rinsing off. - Green tea extract:
Green tea is rich in antioxidants that can protect the skin and may help reduce hyperpigmentation. Brew green tea and apply the cooled extract to the affected areas using a cotton ball. - Apple cider vinegar:
Apple cider vinegar has natural acidic properties that can help exfoliate the skin and lighten dark spots. Dilute apple cider vinegar with water and apply it to the pigmented areas using a cotton ball. Rinse off after a few minutes. - Cucumber:
Cucumber has cooling and soothing properties that can benefit the skin. Apply cucumber slices or cucumber juice to the affected areas for 15-20 minutes before rinsing off. - Oatmeal:
Oatmeal has gentle exfoliating properties that can help remove dead skin cells and improve skin texture. Create a paste by mixing oatmeal with yoghourt or milk and apply it to the skin for 15-20 minutes before rinsing off.
How can proper diet prevent skin pigmentation
Proper diet plays a crucial role in maintaining skin health and may contribute to preventing certain skin pigmentation issues. A balanced and nutritious diet can provide essential vitamins, minerals, antioxidants, and other nutrients that support skin function, repair, and overall radiance.
- Antioxidant-rich foods:
Antioxidants help neutralise free radicals, which are unstable molecules that can damage skin cells and lead to premature aging and skin pigmentation issues. Include foods rich in antioxidants, such as berries (blueberries, strawberries, raspberries), citrus fruits (oranges, lemons), leafy greens (spinach, kale), and colourful vegetables (carrots, tomatoes, sweet potatoes) in your diet. - Vitamin C:
Vitamin C is essential for collagen synthesis and plays a crucial role in skin health. It can help reduce hyperpigmentation and promote a more even skin tone. Foods high in vitamin C include citrus fruits, bell peppers, kiwi, guava, and broccoli. - Vitamin E:
Vitamin E is an antioxidant that helps protect the skin from damage caused by UV radiation and environmental stressors. Nuts (almonds, sunflower seeds), seeds, spinach, and avocados are good sources of vitamin E. - Beta-carotene:
Foods rich in beta-carotene, a type of antioxidant and precursor to vitamin A, can help protect the skin from sun damage and improve skin health. These include orange and yellow fruits and vegetables, such as carrots, mangoes, and sweet potatoes. - Omega-3 fatty acids:
Omega-3 fatty acids have anti-inflammatory properties and help maintain skin moisture and elasticity. Include sources of omega-3s in your diet, such as fatty fish (salmon, mackerel, sardines), flaxseeds, chia seeds, and walnuts. - Zinc:
Zinc is essential for skin repair and wound healing. It also helps protect the skin from UV radiation. Foods high in zinc include whole grains, legumes (beans, lentils), nuts, seeds, and dairy products. - Hydration:
Staying well-hydrated is vital for maintaining skin health and preventing dryness or flakiness that can exacerbate pigmentation issues. Drink plenty of water and consume hydrating foods like cucumbers, watermelon, and celery. - Avoiding triggers:
Some individuals may have specific triggers in their diet that exacerbate skin conditions like acne, rosacea, or eczema, which can lead to post-inflammatory hyperpigmentation. Keeping track of these triggers and avoiding them can help prevent skin pigmentation issues. - Moderate sugar and processed foods:
High intake of sugar and processed foods can cause inflammation in the body, potentially impacting the skin. Reducing the consumption of these foods may benefit skin health.
When to consult a doctor for skin pigmentation issues?
Consulting a doctor for skin pigmentation issues is essential if you notice any persistent or concerning changes in your skin’s pigmentation. While some pigmentation changes may be harmless, others could be indicative of underlying medical conditions or skin disorders that require proper evaluation and treatment.
- New or changing moles:
If you notice new moles or existing moles that have changed in size, shape, colour, or texture, it’s crucial to consult a doctor. These changes could be signs of melanoma, a potentially dangerous form of skin cancer. - Dark spots or patches:
If you have developed dark spots or patches on your skin that are not related to sun exposure and do not fade over time, a medical evaluation is necessary. These could be signs of conditions like melasma, post-inflammatory hyperpigmentation (PIH), or other pigmentation disorders. - Sudden appearance of white patches:
The sudden appearance of white patches on the skin, especially in areas with no history of injury or sunburn, may be indicative of conditions like vitiligo. A dermatologist can diagnose and manage such conditions. - Itchy, painful, or inflamed skin lesions:
If you have pigmented skin lesions that are accompanied by itching, pain, inflammation, or oozing, consult a doctor promptly. These symptoms may indicate an infection or an allergic reaction. - Persistent pigmentation changes:
If you have tried over-the-counter treatments for pigmentation issues, and there is no improvement or the condition worsens, it’s time to seek professional advice. A dermatologist can provide a proper diagnosis and recommend appropriate treatments. - Pigmentation changes after medication use:
If you notice pigmentation changes after starting a new medication, discuss this with your doctor. Some medications can cause pigmentation issues as side effects. - Pigmentation changes with hormonal changes:
If you experience pigmentation changes during pregnancy or while taking hormonal medications, it’s essential to consult a healthcare professional. Conditions like melasma can be hormonally induced and may require specific management. - Concerns about skin cancer:
If you are concerned about the possibility of skin cancer or have a family history of skin cancer, it is wise to have regular skin check-ups by a dermatologist, especially if you notice any abnormal skin pigmentation.
Skin pigmentation treatment options
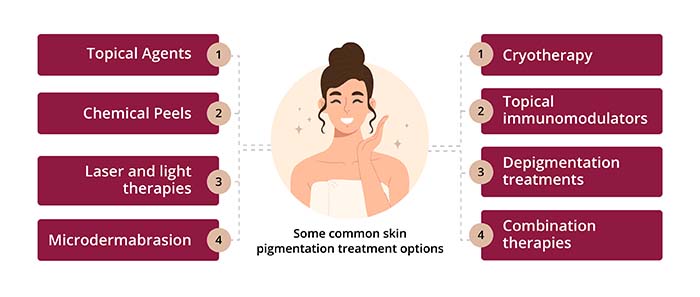
Skin pigmentation treatment options vary depending on the type and severity of the pigmentation issue. Some treatments focus on lightening dark spots, while others aim to repigment areas of hypopigmentation. It’s essential to consult with a dermatologist to determine the most suitable treatment for your specific condition.
Some common skin pigmentation treatment options:
- Topical Agents:
- Hydroquinone:
Hydroquinone is a skin-lightening agent that can be effective for treating hyperpigmentation. It works by inhibiting the production of melanin. Over-the-counter products typically contain lower concentrations (2%) of hydroquinone, while higher strengths (up to 4%) are available by prescription. - Retinoids:
Retinoids, derived from vitamin A, can help improve skin texture and reduce pigmentation issues. They work by increasing cell turnover and promoting the fading of dark spots. - Vitamin C serums:
Topical vitamin C serums can help brighten the skin and reduce hyperpigmentation due to their antioxidant properties and ability to inhibit melanin production. - Kojic acid:
Kojic acid is a natural skin-lightening agent derived from certain fungi. It can be used to treat hyperpigmentation and is often found in combination with other lightening agents.
- Hydroquinone:
- Chemical Peels:
Chemical peels involve the application of a chemical solution to the skin, which exfoliates the top layer of skin and promotes skin regeneration. Chemical peels can improve the appearance of hyperpigmentation and promote a more even skin tone. - Laser and light therapies:
- Intense pulsed light (IPL) therapy:
IPL uses broad-spectrum light to target areas of hyperpigmentation, effectively breaking down the excess melanin and promoting skin rejuvenation. - Fractional laser therapy:
Fractional lasers target specific areas of the skin, creating controlled micro-injuries that stimulate collagen production and help even out skin tone. - Q-switched laser:
Q-switched lasers emit high-energy pulses that break down pigment particles, making them suitable for treating specific types of hyperpigmentation, such as sunspots and freckles.
- Intense pulsed light (IPL) therapy:
- Microdermabrasion:
Microdermabrasion involves exfoliating the outer layer of skin using fine crystals or a diamond-tipped device. This procedure can improve the appearance of hyperpigmentation and promote skin renewal. - Cryotherapy:
Cryotherapy involves freezing the pigmented areas with liquid nitrogen, causing the skin to peel off, and promoting the growth of new, healthier skin. - Topical immunomodulators:
For certain types of hypopigmentation, topical immunomodulators may be prescribed to stimulate the repigmentation process. - Depigmentation treatments:
In some cases, individuals with extensive vitiligo may opt for depigmentation treatments to lighten the unaffected skin and achieve a more even appearance. - Combination therapies:
Dermatologists may recommend combining different treatments for more effective results, especially for complex pigmentation issues.
Additionally, proper sun protection and skincare practices are essential during and after treatment to maintain the improvements achieved. A dermatologist can guide you in selecting the best treatment option based on your individual needs and skin type.





